In 1963, writer Aldous Huxley was on his deathbed suffering from terminal cancer when he asked his wife to inject him with 100 micrograms of LSD. In a letter to friends, Laura Huxley wrote that she consulted Sidney Cohen, a psychiatrist who had pioneered the use of LSD. “I had asked him if he had ever given LSD to a man in this condition. He said he had only done it twice, actually,” wrote Laura, “and in one case it had brought up a sort of reconciliation with death.”
After the author of “The Doors of Perception” and “Brave New World” passed away, Laura wrote, “All five people in the room said that this was the most serene, the most beautiful death. Both doctors and the nurse said they had never seen a person in similar physical condition going off so completely without pain and without struggle.” Three years later, LSD was officially banned in California.
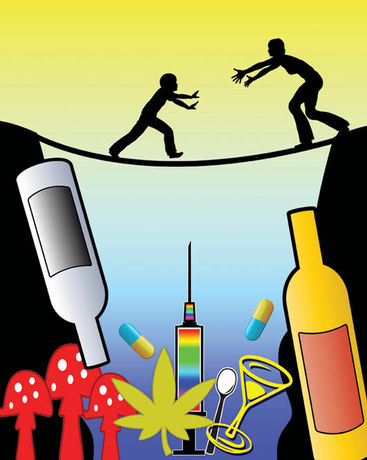
Much has been recently discussed on the use of psychedelics for the treatment of many conditions, including its therapeutic administration for PTSD, depression, alcohol or hard drug abuse, couples’ therapy, anxiety and more. The focus is on healing and recovery from traumas and unresolved grief. Less is known about utilizing these same entheogens for those with terminal illnesses – for palliative care during the end of life experience.
I spoke with Dr. Alison Draisin PsyD, LMHC, lead psychotherapist and Director of Ketamine Assisted Psychotherapy Provider Training at the AIMS Institute, to discover more about her knowledge of Cannabis and psychedelics as a tool in psychotherapy, and in particular, for patients who are preparing for their deaths. “End of life therapy using these plant and fungal medicines isn’t about healing and recovery, but instead about acceptance, pain management and feeling peace within themselves,” explains Dr. Draisin. “The spiritual awakenings can be quite cathartic for the patients and observing their experiences has brought me peace as well. It’s so lovely and powerful to bear witness to people’s journeys to discover death with peace.”
Dr. Draisin also tells me that The AIMS Institute, short for Advanced Integrative Medical Science, employs ketamine for patients in palliative care and recently sued the DEA in order for them to allow psilocybin treatments for those in hospice. Lawyer Kathryn Tucker of the Emerge Law Group filed a motion on behalf of AIMS clients pushing for rescheduling, but the judge came back and said the DEA has no precedent.
“It’s a catch-22 because without the right to use mushrooms for patients, there’s no studies to show efficacy – and the DEA can just point to that and continue to stonewall any rescheduling by citing the fact that there’s no evidence.” After the lawsuit was rejected, the company Dr. Bronner’s Magic Soaps sponsored a protest on behalf of Right to Try at the DEA building in Arlington to raise awareness of the fact that the agency was blocking the implementation of the Right to Try Act passed and signed into law in 2018.
According to the Act: “Psilocybin therapy has shown incredible promise alleviating the debilitating existential distress many terminally ill Americans face in their last days, sabotaging their quality of life and time with family and friends. FDA has granted “breakthrough status” to psilocybin therapy for depression, in light of safety and promising signs of efficacy in stage 2 FDA trials, especially for end of life patents. Congress passed the national Right to Try Act in 2018 to allow Americans with life-threatening conditions to access promising medicines that have passed phase I trials, without having to wait for completion of the new drug approval process. However DEA is blocking access to psilocybin therapy, even as Canada is now allowing it north of the border.”
In a recent opinion piece in the New York Times, health and science writer and former psychology researcher Dr. Dana G. Smith writes about Nick Fernadez, who was administered “a large dose of psilocybin as part of a clinical trial at New York University for people dealing with anxiety and depression following a cancer diagnosis.” Mr. Fernandez wrote about his experience in a Medium post, describing what many would consider to be a miracle. “This psilocybin journey was the single most transformative experience of my life,” he explained. “It forced me to reconcile with the mortality of being human. It alleviated my anxiety and gave meaning to my life.”
How do we get to a future in which dying human beings are able to choose for themselves the treatments they wish to employ? Does “Death with Dignity” include the right to use psychedelics to help come to terms with the end of our lives in a truly “Brave New World?” As Dr. Draisin sees it, the answers are obvious.
“We’re still fighting and we need more people to become activists and be public about their support for these end-of-life therapies,” she says. “It’s hard because the people who need this the most aren’t able to keep up the fight but their loved ones – and anyone who believes in this right – need to step up. People who are dying deserve the right to do whatever they want with their bodies and minds.”
Resources for Activists and Patients
AIMS Institute – aimsinstitute.net
End Well Project – endwellproject.org
Right to Try Psilocybin – righttotrypsilocybin.com
Dr. Bronner’s – drbronner.com/blogs/our-community/heal-soul
WAMM (Wo/Men’s Alliance for Medical Marijuana) – wammphytotherapies.org
End of Life Washington – endoflifewa.org
The Johns Hopkins Center for Psychedelic and Consciousness Research – hopkinspsychedelic.org
Nushama (Ketamine Assisted Therapy Clinics) – nushama.com
The Heffter Research Institute – heffter.org
TheraPsil (Canada) – therapsil.ca
Center to Advance Palliative Care – capc.org